|
October 2013
|
October 2013 // Volume 51 // Number 5 // Feature // v51-5a9
The Prize Is Healthy Eyes: Using Games to Educate About Diabetic Retinopathy
Abstract
This article describes a program for prevention of diabetic retinopathy (DR) that was designed for Extension in collaboration with optometrists. The program was created to increase knowledge and awareness about risk factors for DR and included a game and take-home materials. Participants were asked to play a game similar to Wheel of Fortune. A total of 89% of questions were answered correctly. A telephone survey was used to track retention of knowledge and revealed that participants had used increased knowledge to make positive lifestyle changes. Of individuals who participated in the interactive game, measurable improvements in knowledge and awareness occurred.
Introduction
According to the Centers for Disease Control and Prevention (CDCa, 2008), diabetes is the seventh leading cause of death in the United States (CDCa, 2008). Prevalence of diagnosed and undiagnosed diabetes is estimated at 23.6 million people (7.8% of the U.S. population) (CDCa, 2008) and is expected to double by 2031 (Huang, Basu, O'Grady, & Capretta, 2009). Of the various ethnic groups, American Indians and Alaska Natives have the highest rates of diabetes (16.5%) (CDCa, 2008). By 2030, the number of older persons (aged 65 and older) is expected to increase to 20% of the population; currently, one fifth of those aged 60 and older are diagnosed with diabetes (Administration on Aging, 2012). While approximately 57 million people currently have pre-diabetes in the U.S. (CDCb, 2008), worldwide, experts predict prevalence to grow to 470 million by 2030 (Administration on Aging, 2012). Direct and indirect medical costs of diabetes in the U.S. are estimated at $174 billion (CDCa, 2008).
Ramifications of uncontrolled diabetes include:
- Heart disease
- Stroke
- High blood pressure
- Blindness
- Kidney failure
- Nervous system damage
- Amputations
- Dental disease
- Pregnancy complications
- Increased susceptibility to illness
- Decreased functional capacity (ability to work)
Complications of diabetes can be decreased by receiving preventive care in a timely manner and by controlling (CDCa, 2008):
- Blood glucose levels
- Blood pressure
- Blood lipids
Diabetic retinopathy (DR), a diabetic eye disease, accounts for 12,000 to 24,000 new cases of blindness every year and is the leading cause of new cases of blindness in adults (American Diabetes Association, 2007; CDCa, 2008). DR is seen in 40 to 45% of Americans diagnosed with diabetes (Ammary-Risch & Huang, 2011). Vision loss can be reduced by 50-60% with the detection and treatment of diabetic eye disease and with laser therapy (CDCb, 2008).
As the prevalence of diabetes continues to increase, those affected by diabetic complications such as DR tends to increase. Because DR may be accompanied by no symptoms, healthcare providers, as well as those with diabetes or pre-diabetes, need to be aware of the disease and how to prevent and treat it. Vision loss and blindness can be prevented through early detection of DR, but many patients seek care at a "point of no return," and treatments are, at this point, limited (Ammary-Risch & Huang, 2011). Preventive care (e.g., annual dilated eye examinations, smoking cessation programs) and a healthful diet have been shown to be effective in decreasing diabetic complications and represent the only standard of care for early onset DR; however, they are underutilized (Adams, & Bearse, 2012). In a survey of minority primary care physicians, slightly more than half (52%) indicated that they have adequate knowledge to advise their diabetic patients on eye health (Ammary-Risch, & Huang, 2011). Prevention programs focused on DR and diabetes should be widely offered and include tips for diet, eye care, and other lifestyle intervention components.
Extension educators note that knowledge is a vital first step to motivate change in diet (Chapman-Novakofski, DeBruine, Derrick, Karduck, Todd, & Todd, 2004). An educational program, Eating for Your Eyes: Diabetic Retinopathy Prevention, Treatment and Diet, was developed to increase knowledge regarding preventive care and diet for individuals at risk for DR. An interactive game was created, along with an educational display poster and take-home brochure, to increase awareness and knowledge of the importance of screening for and prevention of DR in individuals at risk for DR, particularly among older adults and American Indians. Like other Extension diabetic education programs, this program includes collaborations with community partners, is designed to reach low-income older adults with diabetes or at risk for diabetes, and includes a plate method teaching guide (Corbin, Kiernan, & Gettings, 2007; Williams, LeBlanc, & Christensen, 2004, respectively). Also, the program uses the same model as other effective Extension programs, because it creates learning partnerships that empower adults to enhance their lives, specifically in the area of eye health and nutrition education (Stastny & Garden-Robinson, 2011). The novelty of the DR program is in its teaching approach: to pique interest in nutrition education by emphasizing vision health—a key concern for the older adult and American Indian population. The effectiveness of the educational program was evaluated.
Subjects and Methods
Eating for Your Eyes: Diabetic Retinopathy is structured for use with specific demographic groups that are especially at risk for diabetes: American Indians and older adults. The program was piloted at an optometric annual meeting. Following final program review and Institutional Review Board (IRB) approval, the program was offered to individuals attending pow wows (gathering of North America's native people), health fairs, and similar public events that included other exhibitors along with the current program. Educators included county Extension agents and university dietetic students, each working alone in different parts of the state.
The program consisted of an interactive, engaging booth offered at health fair-type venues. Participants were asked to play a game similar to the television game show, Wheel of Fortune, and to answer two flash card questions correctly. Operated by the participants, the game wheel included colorful game pieces and a familiar clicking noise. Each game piece was color coded with visual graphics to indicate which question category to ask the participant. Figure 1 shows a photograph of the poster and game wheel.
Figure 1.
Game Wheel and Poster with Dietetic Student Educator
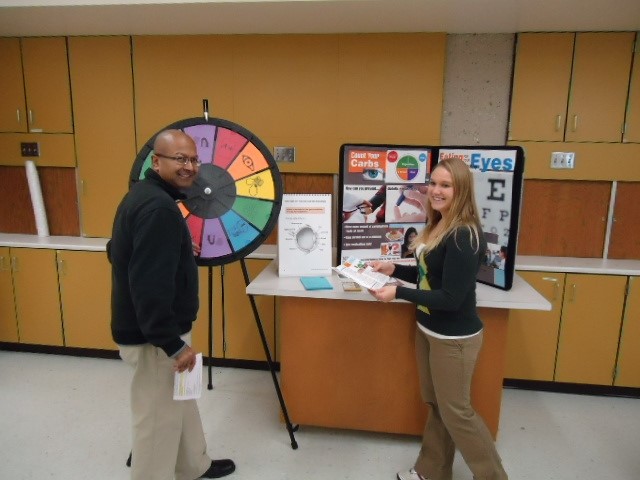
Unlike the handcrafted Wheel of Fortune designed by Morgan-Coures (1983), the game wheel presented here was purchased online and was easily assembled in less than 1 hour. The research assistant, i.e., educator, was equipped with card stock flash cards printed with two questions back to back on color aligned paper: true/false (T/F) on one side and multiple-choice on the other. Besides the quick game of answering two questions, the educator had the option of asking participants to participate in a more in-depth, slightly longer pre- and post-survey. In addition, educators had the opportunity to provide the participants, on a broader scope, with information related to food model portion recommendations and food preparation ideas to prevent or control diabetes and DR, plus other lifestyle recommendations for prevention of DR.
Spreadsheets were created to record correct/incorrect responses to the game. For correct answers, participants were given a "prize," an "Eating for Your Eyes pill/vitamin organizer." They also were encouraged to share the DR information with others. For incorrect answers, educators assisted the participants to find the correct answer on the poster, and the participants also received a "prize." All participants were provided an easy-to-understand professionally designed brochure that was created by an Extension dietitian/gerontologist team and peer-reviewed by optometrists, certified diabetes educators, and an ophthalmologist.
Additionally, each participant who indicated risk for diabetes was given a reminder card to schedule a dilated eye exam within the next year. The reminder card, designed by the state optometric association, encourages information sharing among the participant, the participant's primary care physician, and eye health professional.
The pre- and post-survey included the collection of demographic and, optionally, contact information. Matched questions from the post-survey were used in a follow-up telephone survey 1 month after the program, and a telephone script was used to assure consistent delivery. Data entry was accomplished using an Excel spreadsheet while the call was in progress. Questions on the telephone survey were identical or closely matched to game questions, to compare retained knowledge and awareness about DR.
Statistical Analysis
Frequencies for the initial number of correct and incorrect answers to the 12 game questions were tabulated for the tribal communities group (3 sites), and the community centers group (4 sites), as well as for the combined tribal and community center groups (7 sites). Using Chi square, the goodness of fit for correct answers was compared to normal for each subset of tribal communities, community center groups, and the two combined groups (tribal community/community centers). One of the tribal health fair sites had fewer than five completed question sets (one T/F; one multiple choice), so this data was not included in Chi square testing. Regardless of category, we assumed that participants had a 50:50 chance of correctly answering a T/F question and a 25% chance of answering one of the multiple choice questions correctly (4 choices, single answer), due to chance alone. We would also expect that a participant would answer both the T/F question and the multiple choice questions correctly within each category 12.5% of the time, due to chance alone. SAS version 9.2 was used to calculate the Chi squares, based on predicted percentages and actual percentages (SAS Institute, Cary, NC, 2009). Data was analyzed using SPSS version 17.0 (SPSS, Inc., Chicago, IL, 2009). For all data, level of significance was set at P≤0.05.
Results/Findings
The educational activity was offered to 246 participants at senior centers, diabetic clinics, health fairs, pow wows, and community building gatherings. Table 1 shows the categories for the questions.
| Green | Plate Method for Improving Portion Control |
| Blue | Which Are Carbohydrate Foods? |
| Orange | How is Diabetic Retinopathy Related to Blindness? |
| Purple | Importance of Dilated Eye Exam |
| Red | Risk Factors for Diabetic Retinopathy |
| Yellow | How Can You Prevent Diabetic Eye Disease? |
Statistics in Table 2 show the differences between expected and actual values for numbers of correct answers to the questions for the different categories.
| Tribal Groups n=122 | Community Groups n=116 | Both Groups Combined n=238 | |
| Question Categories: | Chi square (p value) | Chi square (p value) | Chi square (p value) |
| Blue | 11.33 (0.01) | 58.10 (<0.0001) | 62.16 (<0.0001) |
| Green | 21.33 (<0.0001) | 57.21 (<0.0001) | 75.02 (<0.0001) |
| Orange | 70.0 (<0.0001) | 72.27 (<0.0001) | 145.56 (<0.0001) |
| Purple | 55.07 (<0.0001) | 103.06 (<0.0001) | 157.99 (<0.0001) |
| Red | 26.88 (<0.0001) | 102.96 (<0.0001) | 124.76 (<0.0001) |
| Yellow | 29.33 (<0.0001) | 63.4 (<0.0001) | 91.2 (<0.0001) |
Results by Flash Card Question Color Category
- Orange: The highest Chi squares were calculated for the orange category questions (70.0, p<0.0001) within the tribal community, where there were no incorrect answers. The orange category questions, which focused on DR and blindness, were most frequently answered correctly; overall, 94% of participants answered questions correctly. Among community center participants and combined tribal community participants, 93% and 95%, respectively, answered the orange category "DR and blindness" questions correctly.
- Purple: Purple category questions highlighted the importance of not only having an annual eye exam if at risk for diabetes, but also the importance of having a dilated eye exam, when having an exam. Chi squares (and correct answers) were highest for the purple category questions in the community centers (103.06, p<0.0001); and overall (157.99, p<0.0001).
- Red: Risk factors for DR made up the content for the red category questions. The red category questions also had higher Chi square values, relative to other colors for the overall groups (124.76, p<0.0001) and for the community groups (102.96, p<0.0001) but not as high for the tribal groups (26.88, p<0.0001).
- Yellow: The yellow category questions, included knowledge about "how can you prevent DR" such as controlling blood pressure, sugar, lipids, and having a dilated eye exam. The probabilities that the yellow category questions were answered correctly, not necessarily by chance alone showed mixed results, all significant.
- Blue and Green: The blue and green category questions seemed to be the most difficult for participants regardless of venue. Even in the pilot testing with optometrists at a conference, the green category questions were answered correctly the least times. The green category questions asked the correct number of carbohydrate foods to include in a meal using the USDA MyPlate icon (USDA, 2010) and whether or not it is a helpful tool for portion control. Others have found difficulty with identification of carbohydrate foods in Extension programs (Chapman-Novakofski et al., 2004). Blue category questions were related to carbohydrate-containing foods and queried the participants whether those diagnosed with diabetes should eat fruit. None of the participants answered the blue category questions incorrectly during the pilot testing; however, at the community sites, 8 of 26 participants did not know or were unsure which of the following contained the most carbohydrate per serving: (a) milk and yogurt; (b) meat, fish and poultry; (c) watery vegetables; or (d) butter, margarine and oil.
Post- and Telephone Follow-up Survey Results
Of the 61 participants who provided contact information, 24 participated in a post-telephone interview. The interview included a post-survey that included questions about participants' current diet-related behaviors. A total of 89% of the post-survey questions were answered correctly. Participants' responses to follow-up questions revealed the following results.
- 67% of participants shared the information learned with someone else.
- 75% of participants increased physical activity.
- 96% prepared meals including vegetables more often.
- 92% included protein with each meal.
- 71% tried to have a consistent amount of carbohydrates per meal.
Discussion and Recommendations
During Eating for Your Eyes: Diabetic Retinopathy program offerings at three pow wows and five community centers, 246 people were reached. A high number of correct answers to the DR questions were demonstrated, which shows that even short educational programs can make an impact in increasing knowledge and awareness. Participants seemed to be receptive to information regarding DR and the importance of having a dilated eye exam. Understanding portion control, how much carbohydrate foods to eat, and what makes up a carbohydrate food were challenging topics for the participants in this study.
Individual beliefs regarding complications of diabetes can have a positive impact on lifestyle behaviors that affect later outcomes of the disease (Rees, Sasongko, Fenwick, Nicolaou, Wong, & Lamoureux, 2012). The follow-up telephone survey probed participants to indicate their level of learning during the program and to determine participants' intentions for using the information in their daily lives. Based on the application of Social Cognitive Theory in this context, individuals continue to learn across the lifespan and can retain information from a short educational program to make positive lifestyle changes (Bandura, 1989). For the most part, both older adult and American Indian participants seemed to understand that those who are at risk for diabetes also are at risk of losing their sight; however, lifestyle changes such as diet and exercise (i.e., changes that can prevent one from getting diabetes and DR) posed more of a challenge. DR education should contain a component for diet, or perhaps a referral to a session that focuses on diet and other lifestyle behaviors (e.g., knowing blood pressure, blood sugar, and blood lipid personal numbers). In addition, all diabetic education programs should include reminders about the importance of dilated eye exams.
Eating for Your Eyes: Diabetic Retinopathy alerted individuals to the importance of lifestyle behavior changes such as control of blood sugar, blood lipids, and blood pressure, and having regular dilated eye exams to maintain healthy eyes. As a result of the education, the participants may feel empowered to prevent diabetic complications. Because many physicians felt that they did not have adequate knowledge to advise their diabetic patients on eye health, it is imperative that DR education programs systemically refer those at risk for diabetes to:
- An optometrist or ophthalmologist for a dilated eye examination
- A diabetic educator to learn about portions and recommended eating plans.
The eye exam referral cards and take-home brochure are helpful to start the referral process. Extension diabetic education programs such as the program described here and by others (Grenci, 2010) reach not only the individual, but also family members and other professionals such as social services personnel who serve clients with diabetes. Reminders to get an eye exam can be initiated by a variety of stakeholders.
Outcome data such as numbers of individuals at risk for diabetes that actually receive an annual dilated eye exam are difficult to collect; however, the Eating for Your Eyes team is working with service groups such as Lions International to increase numbers of individuals that can help implement the program objectives.
Treatments for DR are limited, are only somewhat effective, and can be invasive to some extent (Adams & Bearse, 2012). On the Reservation sites, and in other rural areas, access to laser treatments is sparse and may entail driving hundreds of miles for individual treatments. Eye disease takes away from productivity in the workplace and from quality of life. As a complication of diabetes, DR is less easily corrected in older adults relative to younger individuals (Bloomgarden, 2007). Prevention of DR is critical.
Implications and Conclusion
With age, the risk for having diabetes and subsequent DR increases (Administration on Aging, 2012). The proportion and numbers of older adults at risk for chronic disease such as diabetes are growing in the U.S. and worldwide (Administration on Aging, 2012). Considering all ethnicities studied, American Indians are one of the groups at greatest risk for diabetes (CDCb, 2008). DR prevention and educational programs should include information about nutrition and its impact on DR prevention. Because signs and symptoms of diabetic eye disease are not easily noticed among those with early DR, educational programs should include descriptions and reminders about the importance of dilated eye exams and other lifestyle precautions for those at risk for diabetes.
Of the small sample of individuals who participated in Eating for Your Eyes, measurable improvements in knowledge and awareness related to DR occurred. The program, using an interactive display typical of community-based Extension programming, influenced knowledge and potential lifestyle behavior change for both older adult and American Indian participants.
Health professional confidence in screening for and detection of diabetic eye disease is needed and warranted. The Eating for Your Eyes: Diabetic Retinopathy program has promoted behavior change and is easily replicated. The educational brochure is available at http://www.ag.ndsu.edu/pubs/yf/foods/fn1493.pdf and use of materials from the program is encouraged by others. North Dakota State University Extension plans to use the wheel for a variety of future nutrition education programs. In North Dakota, we encourage each county to borrow the wheel and have therefore purchased a second wheel to increase offerings.
Acknowledgments
This project was partially funded by a Healthy Vision Community Award from the National Eye Institute in collaboration with the North Dakota Optometric Association. Lindsay Youd, MS, RD, former North Dakota State University graduate assistant assisted with literature review as part of her thesis; Nicole Seaberg, pictured, assisted with data collection; Jamie Kubat, North Dakota State graduate assistant, assisted with the data analysis.
References
Adams, A. A., & Bearse, M. A. (2012). Retinal neuropathy precedes vasculopathy in diabetes: A function-based opportunity for early treatment intervention? Clinical and Experimental Optometry, 95, 256-265. doi: 10.1111/j.1444-0938.2012.00733.x
Administration on Aging (2012). Aging statistics. Retrieved from: www.aoa.gov/aoaroot/aging_statistics/index.aspx
American Diabetes Association (2007). Standards of medical care in diabetes. Diabetes Care, 30, S1, S21-S41.
Ammary-Risch, N. J., & Huang, S. S. (2011). The primary care physician's role in preventing vision loss and blindness in patients with diabetes. Journal of the National Medical Association, 103, 281-283.
Bandura, A. (1989) Six theories of childhood development. In R. Vastal Ed., Annals of childhood development (1-60). JAI Press, Greenwich, Connecticut,
Bloomgarden, Z. (2007). Screening for and managing diabetic retinopathy: Current approaches. American Journal of Health Systems Pharmacy, 17, S8-S14. doi: 10.2146/ajhp070331
Centers for Disease Control and Prevention [CDCa]. (2008). National diabetes fact sheet: General information and national estimates on diabetes in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Retrieved from: http://apps.nccd.cdc.gov/DDTSTRS/FactSheet.aspx
Centers for Disease Control and Prevention [CDCb]. (2008). Estimates of diagnosed diabetes now available for all U. S. counties. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Retrieved from: http://www.cdc.gov/media/pressrel/2008/r080624.htm?s_cid=mediarel_r080624
Chapman-Novakofski, K., DeBruine, V., Derrick, B., Karduck, J., Todd, J., & Todd, S. (2004). Using evaluation to guide program content: Diabetes education. Journal of Extension [On-line], 42(3) Article 3IAW1. Available at: http://www.joe.org/joe/2004june/iw1.php
Corbin, M., Kiernan, N. E., & Gettings, M. A. (2007). Preventing diabetes: You have the power to take action. Journal of Extension [On-line], 45(5) Article 5FEA5. Available at: http://www.joe.org/joe/2007october/a5.php
Grenci, A. (2010). Applying new diabetes teaching tools in health-related extension programming. Journal of Extension [On-line], 48(1) Article 1IAW5. Available at: http://www.joe.org/joe/2010february/iw5.php
Huang, E. S., Basu, A., O'Grady, M., & Capretta, J. C. (2009). Projecting the future diabetes population size and related costs for the U.S. Diabetes Care, 32, 2225-2229. doi: http://dx.doi.org/10.2337/dc09-0459
Morgan-Coures, H. J. (1983). Idea corner: Using a "Wheel of Fortune." Journal of Extension [On-line], 21(6). Available at: http://www.joe.org/joe/1983november/83-6-id1.pdf
Rees, G., Sasongko, M., Fenwick, E., Nicolaou, T., Wong, T., & Lamoureux, E. (2012). Impact of diabetic retinopathy on patients' beliefs about diabetes. Clinical and Experimental Optometry, 95, 371-376. doi: 10.1111/j.1444-0938.2012.00745.x
Stastny, S., & Garden-Robinson, J. (2011). Eating for your eyes. Journal of Nutrition Education and Behavior, 43, 137-139.
United States Department of Agriculture (USDA) Dietary Guidelines for Americans (2010). Retrieved from: http://www.choosemyplate.gov/
Williams, D. P., LeBlanc, H., & Christensen, N. K. (2004). Stepping up to the plate: An Education curriculum focused on food portioning skills. Journal of Extension [On-line], 42(3) Article 3RIB7. Available at: http://www.joe.org/joe/2004june/rb7.php