|
August 2018
|
August 2018 // Volume 56 // Number 4 // Research In Brief // v56-4rb1
Latinos Living Well—A Diabetes Education Program for Rural-Residing Latinos
Abstract
Diabetes is a health issue for many Latinos. Extension can help provide diabetes self-management education for rural-residing Latinos. In a pilot study, we evaluated the Extension-delivered diabetes program Latinos Living Well (LLW), as provided to 76 rural-residing Latino adults in a midwestern state. LLW consists of four weekly lessons that include hands-on activities and cooking practicums. Participants completed diabetes self-management, self-efficacy, and knowledge questionnaires; significant (p ≤ .05) changes from before to after the program were detected for each outcome measure. Additionally, participants viewed LLW favorably. Results suggest that LLW is an effective, culturally relevant diabetes self-management education program for Latinos and is appropriate for Extension delivery.
Introduction
Type 2 diabetes mellitus (diabetes) among Latinos is a public health concern. Latinos have a higher diabetes incidence (11.9%) than non-Latino Whites (7.3%) (Centers for Disease Control and Prevention [CDC], 2017). Additionally, 31.7% of Latino adults have prediabetes (CDC, 2017). Despite their higher risk for and incidence of diabetes, 41.3% of Latinos are unaware of their diabetes status (Schniederman et al., 2014).
Several factors place Latinos at higher diabetes risk and severity. First, one third (34.1%) lack health insurance (National Center for Health Statistics, 2017); thus it is likely that physician care, diabetes diagnoses, and referrals to diabetes self-management (DMSM) programs are limited. Second, acculturation influences diabetes risk (O'Brien, Alos, Davey, Bueno, & Whitaker, 2014). As immigrants adopt U.S. cultural practices, diet quality decreases (Perez-Escamilla & Putnik, 2007), potentially leading to weight gain (Oza-Frank & Cunningham, 2010) and thereby raising diabetes risk (Perez-Escamilla & Putnik, 2007). Additionally, rurality may exacerbate diabetes risk due to limited health care access (Meit et al., 2014), less formal education (Hale, Bennet, & Probst, 2010), lower income levels (Hale et al., 2010), fewer physical activity (PA) opportunities (Meit et al., 2014), and limited access to affordable nutrient-dense foods (Smith & Morton, 2009) as compared to the circumstances of those living in urban areas. Furthermore, communication challenges, health illiteracy, discrimination, and mistrust of the health care system place Latinos at a disadvantage for receiving DMSM education (Cristancho, Garces, Peters, & Mueller, 2008). These factors increase diabetes risk and decrease the opportunity to manage it ("Facts about Type 2," 2015; Hu, Amirehsani, Wallace, & Letvak, 2013).
Culturally appropriate DMSM education programs for rural-residing Latinos are needed to help them prevent and/or manage diabetes. Extension is well positioned to fulfill this need as it naturally overcomes several barriers faced by Latinos needing diabetes education. Specifically, it is available nationwide, including in rural areas; is not affiliated with local health care agencies; does not require participants to have health insurance; and can provide diabetes education services for free or at reduced prices.
Latinos Living Well
Latinos Living Well (LLW) is based on two Extension programs, Dining with Diabetes (DWD) ("Dining with Diabetes," 2017) and Kitchen Creations (KC) (Archuleta et al., 2012). DWD improves blood glucose control (Burcham, 2009; "Dining with Diabetes," 2017) and knowledge (Chapman-Novakofski & Karduck, 2005), and KC improves nutrient intake patterns and knowledge (Archuleta et al., 2012). Neither has been examined for the purpose of determining the impact of a multiweek DMSM program on diabetes self-efficacy (DMSE) among rural-residing Latinos.
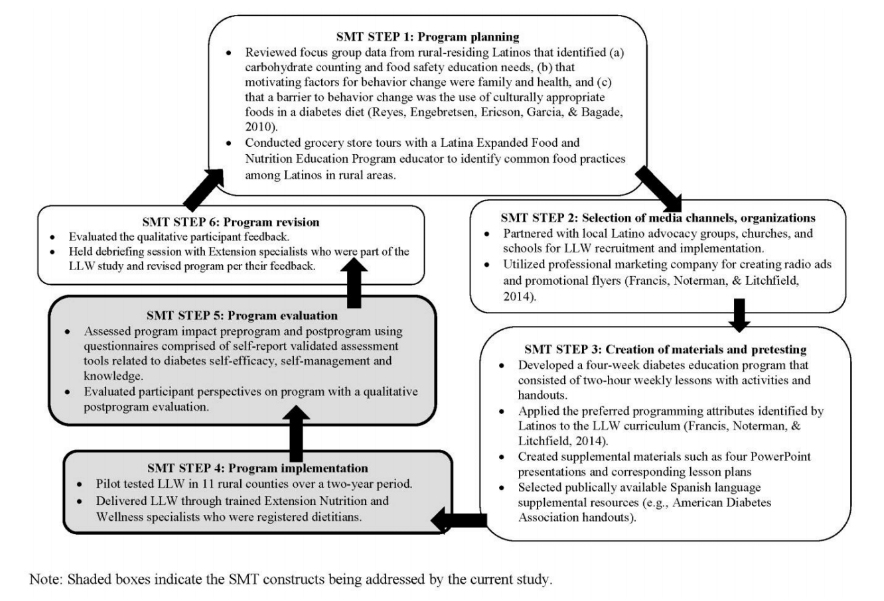
LLW has its foundation in social marketing theory (SMT) (Storey, Saffitz, & Rimón, 2008) and the health belief model (HBM) (Champion & Skinner, 2008). SMT, a program development theory, centers on using the target audiences' needs and preferences to guide program development (Storey et al., 2008). SMT ensures that a program is designed specifically for the target audience, thus increasing the likelihood of program acceptance and success. Figure 1 describes the application of SMT concepts during the development of LLW.
Figure 1.
The Social Marketing Theory (SMT) Process in the Development of Latinos Living Well (LLW)
LLW Description
LLW is a 4-week program delivered in Spanish that focuses on diet and PA for Latinos regardless of diabetes status. The weekly topics are diabetes basics, label reading, beans and vegetables, and fats and sodium. Each lesson includes activities that address at least one HBM construct (Table 1).
| Topic/activity | HBM categories and concepts | ||||||
| Individual perceptions | Likelihood of action | Modifying factors | |||||
| Perceived severity | Perceived susceptibility | Changeable & unchangeable attributes | Cues to action | Self-efficacy | Perceived benefits | Perceived barriers | |
|
Overview of diabetes (Lesson 1) Risk factors Types of diabetes Influence of lifestyle |
X | X | X | ||||
|
Hands-on group activities Carbohydrate counting/label reading (Lessons 1–3) Product taste-testing (Lesson 2) Sugar-free foods Low-fat foods Identifying whole grains (Lesson 2) Cooking practicum (Lessons 2–4) Physical activity break (Zumba) (Lessons 2–4) |
X | X | X | ||||
| Health benefits of eating beans and other vegetables (Lesson 3) | X | X | |||||
|
Motivators and barriers Physical activity changes (Lessons 2–4) Healthful eating and diet changes (Lessons 2–4) Cooking legumes (Lesson 3) |
X | X | X | ||||
| Goal setting (Lessons 1–4) | X | X | |||||
Because LLW is delivered in Spanish, non-Spanish-speaking specialists worked with local interpreters to provide the pilot implementation of the program. Additionally, sessions were led by Extension specialists who were registered dietitians (RDs). LLW lessons are scripted in both Spanish and English to ensure consistent messaging regardless of specialist or interpreter. Specialists attended an LLW training workshop developed and conducted by author team member Sarah Francis. The training addressed Latino-preferred marketing strategies, cross-cultural communication best practices, curriculum review, and cooking practicums.
Methodology
Participants and Recruitment
LLW was implemented in 11 rural Midwest counties. The research protocol was reviewed by Iowa State University's institutional review board and classified as exempt. A convenience sample of 120 rural-residing Latinos aged 18-plus years, regardless of diabetes status, was recruited through (a) collaboration with established Latino-serving community groups, (b) radio commercials aired on local Latino stations, (c) print media, and (d) word of mouth.
LLW was held at locations accessible to participants. Participants received several small items for participating that supported the mission of LLW, such as diabetes education handouts and the cookbook Diabetic Cooking for Latinos (Fuste, 2002).
Program Evaluation
Participants completed a six-page Spanish questionnaire, comprised of several validated tools, at the start of Lesson 1 (preprogram) and at the end of Lesson 4 (postprogram); this took about 45 min.
The Diabetes Self-Efficacy Scale (α = 0.87) measured DMSE with a Likert scale ranging from 1 (not sure at all) to 4 (very sure) that participants used to rate their confidence regarding 10 health-related abilities (Skaff, Mullan, Fisher, & Chesla, 2003). The average of a participant's responses to the 10 questions was calculated, for a final maximum score of 4.
The validated Diabetes Self-Care Activities Measure (Toobert, Hampson, & Glasgow, 2000) assessed DMSM. Participants reported how often they adhered to behaviors in each of three categories: (a) general diet—the frequency of following a personal healthful eating plan; (b) specific diet—eating fruits and vegetables, limiting high-fat foods; and (c) exercise activities (Toobert et al., 2000). For each category, participants identified how many of the preceding 7 days and, on average, how many days per week over the preceding month he or she had adhered to the DMSM activities. The average of a participant's responses to those two questions in each category was calculated, for a maximum score of 7 in each category—general diet, specific diet, and exercise self-care (Toobert et al., 2000).
Knowledge was evaluated via the Diabetes Knowledge Test (α = 0.70) (Fitzgerald et al., 1998). In its original form, this measure contains 10 questions; however, it was modified to exclude two questions not covered by LLW (medication use and blood glucose testing). The revised quiz contained eight multiple-choice questions worth one point each (maximum score = 8).
The preprogram questionnaire also included sociodemographic and diabetes questions, and the postprogram questionnaire included a qualitative program evaluation addressing participants' perceptions of LLW and whether they had made lifestyle changes.
Data Analysis
We analyzed data using the IBM Statistical Package for Social Sciences (SPSS) for Windows version 24.0. Only data for participants with both preprogram and postprogram questionnaires were included in the analysis (n = 76 out of 120; 63.3% completion rate). We tested the influence on completion rate of sociodemographic variables and preprogram DMSM, DMSE, and knowledge scores using crosstabs with chi-square tests. We used descriptive statistics to summarize sociodemographic data, diabetes status, and the qualitative evaluation responses. Finally, we analyzed preprogram-to-postprogram changes in DMSM practices, DMSE, and knowledge using paired-samples t-tests.
Results and Discussion
Participants
Primarily, participants were first-generation immigrants (87.5%), females (97.3%), and aged 30–49 (51.6%) and had at least 9–12 years of education (77.8%) (Table 2). Most (84.7%) were from Mexico (Table 2). The majority of those with diabetes reported having been diagnosed for at least 2 years (Table 2).
| Participant characteristic (number of participants providing a response) | Number | Percentage |
| Gender (75) | ||
| Male | 2 | 2.7 |
| Female | 73 | 97.3 |
| Age (66) | ||
| ≤ 29 years | 15 | 22.7 |
| 30–39 years | 17 | 25.8 |
| 40–49 years | 17 | 25.8 |
| 50–59 years | 12 | 18.2 |
| 60-plus years | 5 | 7.6 |
| Education (71) | ||
| ≤ 8 years | 15 | 21.1 |
| 9–12 years | 3 | 43.7 |
| Some college | 11 | 15.5 |
| College graduate | 14 | 19.7 |
| Acculturation (72) | ||
| 1st generation (born in country other than U.S.) | 63 | 87.5 |
| 2nd generation (born in U.S. with parent from other country) | 9 | 12.5 |
| Country of origin (72) | ||
| Mexico | 61 | 84.7 |
| Central American country | 10 | 13.9 |
| Colombia | 1 | 1.4 |
| Previous diabetes diagnosis | ||
| Gestational diabetes (69) | ||
| Yes | 22 | 31.9 |
| No | 39 | 56.5 |
| Never been pregnant | 8 | 11.6 |
| Prediabetes (69) | ||
| Yes | 11 | 15.9 |
| No | 58 | 84.1 |
| Type 2 diabetes (73) | ||
| Yes | 16 | 21.9 |
| No | 57 | 78.1 |
| Length of time diagnosed with Type 2 diabetes (15)a | ||
| ≤ 1 month | 1 | 6.7 |
| 6 months–1 year | 2 | 13.3 |
| Between 1 and 2 years | ||
| ≥ 2 years | 12 | 80.0 |
| a15 out of 16 with Type 2 diabetes responded. | ||
The completion rate was influenced by gender, with only two of 12 males (16.7%) completing LLW compared to 73 of 104 females (70.2%) (p ≤ .001). This finding is not surprising, as women are more likely than men to use health care services such as nutrition education (De Melo, de Sa, & Gucciardi, 2013; Thompson et al., 2016). No other sociodemographic differences were detected for any of the outcome measures.
DMSM, DMSE, and Knowledge Scores and Qualitative Findings
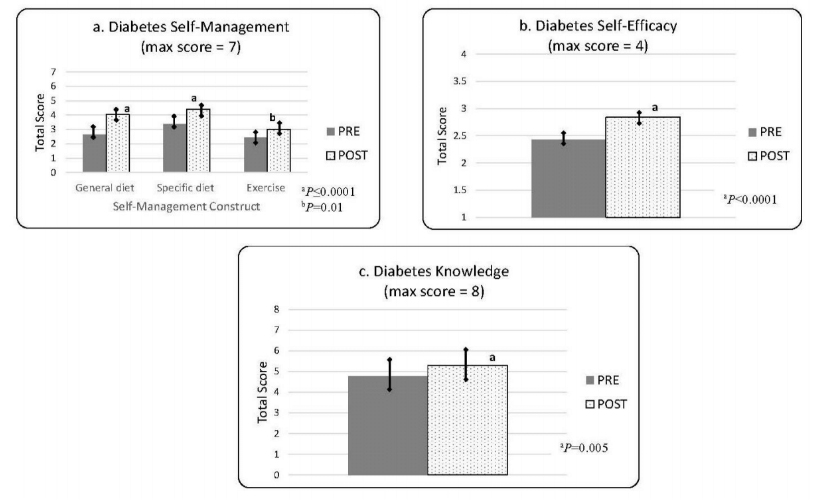
Significant improvements were detected for each outcome measure, and qualitative findings indicated that participants had favorable views of LLW. Specific data are highlighted in the paragraphs that follow; all data are presented in Figure 2 and Table 3 at the end of this subsection.
"General diet" DMSM increased from 2.64±2.18 to 4.04±1.51 (p ≤ .001); "specific diet" DMSM increased from 3.36±1.59 to 4.42±1.28 (p ≤ .001); and "exercise" DMSM improved from 2.44±1.72 to 3.02±1.68 (p ≤ .006) (Figure 2, section a). These changes are promising, as changes in DMSM practices among underrepresented minority groups result in long-term blood glucose control (i.e., hemoglobin A1C) (Ryan, Jennings, Vittoria, & Fedders, 2013). Similarly, Kaiser et al. (2009) found improvements in dietary DMSM following a three-session diabetes intervention among underrepresented minority groups by identifying barriers toward DMSM. Additionally, Archuleta et al. (2012) demonstrated improvements in knowledge and DMSM after a 4-week diabetes intervention with cooking practicums.
The LLW cooking practicums served to introduce participants to healthful, culturally preferred food choices and allowed them to practice food preparation. This program aspect likely empowered participants to choose more healthful food options and prepare more meals that were healthful. This empowerment is also reflected in the qualitative LLW feedback, in which the majority of respondents reported making lifestyle changes during the study (94.5%) and preparing LLW recipes (79.2%) at home (Table 3).
"Exercise" DMSM is likely improved due to the PA breaks that were designed to enhance DMSE and promote discussions of PA benefits and barriers. The LLW PA breaks featured Zumba, a dance-based form of exercise, as dancing helps increase PA in Latinos (Hovell et al., 2008). We chose a publicly available Zumba DVD and Zumba YouTube videos because they indirectly address two common PA barriers reported among Latinos: family responsibilities and limited transportation (D'Alonzo, 2012; Francis, Noterman, & Litchfield, 2014; Parra-Medina & Hilfinger Messias, 2011). The videos could be watched at home (addressing the transportation barrier), and all family members could participate if desired (addressing the family responsibility barrier). This concept is supported by Marcus et al. (2015), who found that home-based exercise interventions improve PA in Latinas over time. Participants likely increased PA as they became more aware of the associated benefits and the strategies for overcoming identified PA barriers. This idea is supported by the qualitative feedback in which the majority of respondents claimed to be more physically active (81.7%) (Table 3). King et al. (2010) reported that PA sessions during diabetes interventions are effective in translating diabetes knowledge into exercise DMSM.
Additionally, DMSE improved from 2.43±.65 to 2.84±.57 (p ≤ .001) (Figure 2, section b), which is very promising as improved DMSE is correlated with improved blood glucose control (Rosal et al., 2011) and predictive of long-term behavior patterns (e.g., PA) (King et al., 2010). The inclusion of multiple skill-based, hands-on, experiential learning activities likely contributed to these changes (King et al., 2010; Rosal et al., 2011). The LLW activities not only taught the needed skills but also helped empower participants to apply the skills outside the classroom.
Finally, knowledge increased from 4.77±1.52 to 5.30±1.65 (p ≤ .004) (Figure 2, section c), suggesting that LLW promoted understanding of diabetes related to lifestyle management. This finding is supported by the qualitative feedback in which the majority (98.6%) reported finding the information to be "understandable" (Table 3). The inclusion of hands-on activities to enhance skill development may have helped participants understand the "why" behind the recommendations and reinforced the "how to" knowledge needed to result in behavior change. This is important, given the lower education levels of the participants.
Nearly all respondents rated LLW as "good" or "excellent" (95.8%) and would recommend LLW to a friend (94.7%) (Table 3). This receptiveness to LLW is also demonstrated by the favorable completion rate. Using target audience feedback (Francis, Noterman et al., 2014; Reyes, Engebretsen, Ericson, Garcia, & Bagade, 2010) better enabled us to ensure that LLW included preferred programming attributes, addressed topics of need, and was scheduled at convenient times for participants and held at trusted locations.
The impact of LLW on DMSM, DMSE, and knowledge is likely attributable to the inclusion of HBM constructs throughout the curriculum. Our results are similar to other successful HBM-based interventions (Archuleta et al., 2012; McClelland, Jayaratne, & Bird, 2013). Furthermore, participants' receptivity to LLW is likely influenced by the SMT-based curriculum, as is the case with other SMT-based interventions (Francis, MacNab, & Shelley, 2014; Francis, Martin, & Taylor, 2011).
Figure 2.
Diabetes Self-Management, Self-Efficacy, and Knowledge Outcomes
| Variable (number of participants providing a response) | Number | Percentage |
| LLW helped me make healthy lifestyle changes (73) | ||
| Agree | 69 | 94.5 |
| Disagree | ||
| Undecided | 4 | 5.5 |
| Prepared at least one class recipe at home (72) | ||
| Yes | 57 | 78.2 |
| No | 15 | 20.8 |
| Added more physical activity to daily routine (71) | ||
| Yes | 58 | 81.7 |
| No | 13 | 18.3 |
| Overall rating of LLW (73) | ||
| Excellent | 55 | 75.3 |
| Good | 15 | 20.5 |
| Needs Improvement | 3 | 4.1 |
| LLW information was understandable (73) | ||
| Agree | 72 | 98.6 |
| Disagree | ||
| Undecided | 1 | 1.4 |
| Would recommend LLW to a friend (72) | ||
| Agree | 72 | 100 |
| Undecided | ||
| Disagree |
Limitations
These results are not generalizable due to our small sample size, sampling methods, and use of self-report data. Although convenience sampling is common practice in Extension, it may have led to the recruitment of Latinos who were more motivated to make behavior changes. The use of self-report surveys was chosen to lessen participant burden during program implementation. However, it presents the possibility for response bias, wherein participants may exaggerate behavior changes to please the program administrators. Lastly, as the participants were primarily females of Mexican descent, the cultural relevance of LLW may be less applicable to men and to those of other Latino cultures.
Implications and Conclusions
LLW provides Extension an opportunity to offer low-cost research-based diabetes education to rural-residing Latinos. Per our cost analysis, it can be offered to 10 participants for approximately $1,600 ($20 weekly per participant). An added benefit is that LLW provides a ready-to-use curriculum complete with training materials, translated scripts, PowerPoint slides, and supplemental materials.
We have found that LLW delivery through Extension is best done via collaborations with Latino-serving community partners. In areas where diabetes education is limited, LLW can be taught collaboratively by a community-based RD or certified diabetes educator (CDE) and the Extension specialist, as is done with DWD. In this delivery model, the RD or CDE leads the diabetes education component while the Extension specialist oversees the cooking and food safety components and cofacilitates the activities. In conclusion, LLW provides the opportunity for Extension to serve the Latino population with culturally appropriate, impactful programming.
Acknowledgments
We gratefully acknowledge the nutrition and wellness specialists from Extension who helped pilot test LLW and revise the curriculum as well as our community partners and Spanish translators. Our work was funded through the U.S. Department of Agriculture, National Institute of Food and Agriculture Rural Health and Safety Education Grant #2014-46100-22349.
References
Archuleta, M., VanLeeuwen, D. Halderson, K., Jackson, K., Bock, M. A., & Eastman, W. (2012). Cooking schools improve nutrient intake patterns of people with type 2 diabetes. Journal of Nutrition Education and Behavior, 44(4), 319–325.
Burcham, L. (2009). Dining with Diabetes: Program helps diabetics make beneficial lifestyle changes. Virginia Tech College of Agriculture and Life Sciences Innovations, 6–7.
Centers for Disease Control and Prevention. (2017). National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services.
Champion, V. L., & Skinner, C. S. (2008). The health belief model. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behavior and health education (4th ed., pp. 45–65), San Francisco, CA: Jossey-Bass.
Chapman-Novakofski, K., & Karduck, J. (2005). Improvement in knowledge, social cognitive theory variables, and movement through stages of change after a community-based diabetes education program. Journal of the American Dietetic Association, 105(10), 1613–1316.
Cristancho, S., Garces, D. M., Peters, K. E., & Mueller, B. C. (2008). Listening to rural Hispanic immigrants in the Midwest: A community-based participatory assessment of major barriers to health care access and use. Qualitative Health Research, 18(5), 633–646.
D'Alonzo, K. T. (2012). The influence of marianismo beliefs on physical activity of immigrant Latinas. Journal of Transcultural Nursing, 23(2), 124–133.
De Melo, M., de Sa, E., & Gucciardi, E. (2013). Exploring differences in Canadian adult men and women with diabetes management: Results from the Canadian Community Health Survey. BMC Public Health, 13, 1089.
Dining with Diabetes. (2017). Retrieved from the West Virginia University Extension Service website: https://extension.wvu.edu/food-health/diabetes/dining-with-diabetes
Facts About Type 2. (2015). Retrieved from http://www.diabetes.org
Fitzgerald, J. T., Funnell, M. M., Hess, G. E., Barr, P. A., Anderson, R. M., Hiss, R. G., & Davis, W. K. (1998). The reliability and validity of a brief diabetes knowledge test. Diabetes Care, 21(5), 706–710.
Francis, S.L., MacNab, L., Shelley, M. (2014). A theory-based newsletter nutrition education program reduces nutritional risk and improves dietary intake for congregate meal participants. Journal of Nutrition in Gerontology and Geriatrics, 33(2), 91–107.
Francis, S. L., Martin, P., & Taylor, K. (2011). Revising an Extension education website for limited resource audiences using social marketing theory. Journal of Extension, 49(6), Available at: http://www.joe.org/joe/2011december/a7.php
Francis, S. L., Noterman, A., & Litchfield, R. (2014). Factors influencing Latino participation in community-based diabetes education. Journal of Extension, 52(5), Article 5RIB5. Available at: https://joe.org/joe/2014october/rb5.php
Fuste, O. (2002). Diabetic cooking for Latinos. Alexandria, VA: American Diabetes Association.
Hale, N. L., Bennet, K. J., & Probst, J. C. (2010). Diabetes care and outcomes: Disparities across rural America. Journal of Community Health, 35(4), 365–374.
Hovell, M. F., Mulvihill, M. M., Buono, M. J., Liles, S., Schade, D. H., Washington, T. A., . . . Sallis, J. F. (2008). Culturally tailored aerobic exercise intervention for low-income Latinas. American Journal of Health Promotion, 22(3), 155–163.
Hu, J., Amirehsani, K., Wallace, D. C., & Letvak, S. (2013). Perceptions of barriers in managing diabetes: Perspectives of Hispanic immigrant patients and family members. Diabetes Education, 39(4), 494–503.
Kaiser, L. L., Martin, A. C., Blackburn, M. L., Metz, D. L., Smith, D., Donohue, S. S., . . . Steinberg, F. M. (2009). Take care of your health! An Extension program to prevent diabetes. Journal of Extension, 47(4) Article 4FEA5. Available at: https://www.joe.org/joe/2009august/a5.php
King, D. K., Glasgow, R. E., Toobert, D. J., Strycker, L. A., Estabrooks, P. A., Osuna, D., & Faber, A. J. (2010). Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care, 33(4), 751–753.
Marcus, B. H., Dunsiger, S. I., Pekmezi, D., Larsen, B. A., Marquez, B., Bock, B. C., . . . Tilkemeier, P. (2015). Twelve-month physical activity outcomes in Latinas in the Seamos Saludables trial. American Journal of Preventive Medicine, 48(2), 179–182.
McClelland, J. W., Jayaratne, K. S. U., & Bird, C. L. (2013). Nutrition education brings behavior and knowledge change in limited-resource older adults. Journal of Extension, 51(4), Article 2FEA1. Available at: https://www.joe.org/joe/2009august/a5.php
Meit, M., Knudson, A., Gilbert, T., Tzy-Chyi Yu, A., Tanenbaum, E., Ormson, E., . . . Popat, S. (2014). The 2014 update of the rural-urban chartbook. Retrieved from https://www.ruralhealthresearch.org/
National Center for Health Statistics (2017). National health interview survey. Retrieved from https://www.cdc.gov/nchs/data/factsheets/factsheet_nhis.htm
O'Brien, M. J., Alos, V. A., Davey, A., Bueno, A., & Whitaker, R. C. (2014). Acculturation and the prevalence of diabetes in US Latino adults, National Health and Nutrition Examination Survey, 2007–2010. Preventing Chronic Disease, 11, E176.
Oza-Frank, R., & Cunningham, S. A. (2010). The weight of U.S. residence among immigrants: A systematic review. Obesity Reviews, 11(4), 271–280.
Parra-Medina, D., & Hilfinger Messias, D. K. (2011). Promotion of physical activity among Mexican-origin women in Texas and South Carolina: An examination of social, cultural, economic, and environmental factors. Quest, 63(1), 100–117.
Perez-Escamilla, R., & Putnik, P. (2007). The role of acculturation in nutrition, lifestyle, and incidence of type 2 diabetes among Latinos. Journal of Nutrition, 137(4), 860–870.
Reyes, J., Engebretsen, B., Ericson, B., Garcia, E., & Bagade, S. (2010). Diabetes focus groups: Report on barriers to chronic illness care. Retrieved from https://www.legis.iowa.gov/docs/publications/IH/13184.pdf
Rosal, M. C., Ockene, I. S., Restrepo, A., White, M. J., Borg, A., Olendzki, B., . . . Reed, G. (2011). Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income Latinos. Diabetes Care, 34(4), 838–844.
Ryan, J. G., Jennings, T., Vittoria, I., & Fedders, M. (2013). Short and long-term outcomes from a multisession diabetes education program targeting low-income minority patients: A six-month follow-up. Clinical Therapeutics, 35(1), A43–A53.
Schniederman, N., Llabre, M., Cowie, C. C., Barnhart, J., Carnethon, M., Gallo, L. C., . . . Aviles-Santa M. L. (2014). Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care, 37(8), 2233–2239.
Skaff, M. M., Mullan, J. T., Fisher, L., & Chesla, C. A. (2003). A contextual model of control beliefs, behavior, and health: Latino and European Americans with type 2 diabetes. Psychology & Health, 18(3), 295–312.
Smith, C., & Morton, L. W. (2009). Rural food deserts: Low-income perspectives on food access in Minnesota and Iowa. Journal of Nutrition Education and Behavior, 41(3), 176–187.
Storey, J. D., Saffitz, G. B., & Rimón, J. G. (2008). Social marketing. In K. Glanz, B. K. Rimer, & K. Viswanath. (Eds.), Health behavior and health education: Theory, research, and practice. (4th ed., pp. 435–464). San Francisco, CA: Jossey-Bass, Inc.
Thompson, A. E., Anisimowicz, Y., Miedema, B., Hogg, W., Wodchis, W. P., & Aubrey-Bassler, K. (2016). The influence of gender and other patient characteristics on health care-seeking behaviour: A QUALICOPC study. BMC Family Practice, 17(38). doi:10.1186/s12875-016-0440-0.
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23(7), 943–950.