|
April 2009
|
April 2009 // Volume 47 // Number 2 // Feature // v47-2a4
Community Health Advisors' Perceptions of the 2005 Dietary Guidelines and MyPyramid
Abstract
This article describes knowledge and
perception of the 2005 Dietary Guidelines for Americans (DG) and
MyPyramid from 106 Community Health Advisors (CHAs) representing
underserved, hard-to-reach communities in Alabama and Mississippi.
Only 16 (15%) were able to correctly identify the MyPyramid graphic
and DG knowledge scores were low. However, most respondents strongly
agreed they would like to know more about the DG (86%) and more
should be done in their community to raise awareness (81%). The
Internet was the least preferred method to communicate DG. More
intense efforts and appropriate communication channels are needed to
promote the DG and MyPyramid.
Introduction
The Expanded Food and Nutrition Education Program's (EFNEP) and the Food Stamp Nutrition Education Program's (FSNEP) use of paraprofessionals has been established as a cost-effective and practical approach for improving the nutritional well-being of disadvantaged populations (Burney & Haughton, 2002; Dickin, Dollahite, & Habicht, 2005; Rajgopal, Cox, Lambur, & Lewis, 2002). A large majority of these paraprofessionals are indigenous to the communities where they work and therefore have a direct understanding of the communities' cultural identity, social networks, and health care needs.
Within some states, the roles of paraprofessionals in EFNEP and FSNEP are essentially seamless with similar job responsibilities, whereas the program roles of EFNEP and FSNEP paraprofessionals vary within other states. However, as evident by recently developed core competencies suggested for FSNEP paraprofessionals, paraprofessionals generally provide an integral role in accessing, assessing, educating, and monitoring vulnerable populations (USDA Cooperative State Research, Education, and Extension Service). Other programs have utilized comparable models, often referred to as community health advisors (CHAs), community health workers (CHWs), or lay health advisors (LHAs) to assess and intervene on a variety of health issues in health disparity populations (Hardy, Wynn, Huckaby, Lisovicz, & White-Johnson, 2005; Jackson & Parks, 1997; Rhodes, Foley, Zometa, & Bloom, 2007). The paraprofessional and other community-based health educator models have tremendous potential to improve access to nutrition-related resources in underserved regions of Alabama's Black Belt and the Lower Mississippi Delta, where accessibility and cultural barriers are common.
The long-term goal of the research targeting rural regions of Alabama's Black Belt and the Lower Mississippi Delta is to develop and implement strategies to promote awareness, knowledge, and adoption of the 2005 Dietary Guidelines for Americans (2005 DG) and the revised Food Guidance System, better known as MyPyramid. Both of these rural regions' populations are predominantly African American with low median incomes, educational achievement, and literacy proficiencies compared to state and national averages (Adult Literacy Estimates, 1996; US Census Bureau). No known published research has explored the degree to which these recently released nutrition recommendations have infiltrated into public access.
As a first step in understanding strategies to promote these new guidelines, we surveyed Community Health Advisors (CHAs) involved in the Deep South Network for Cancer Control (DSNCC). The DSNCC is a project designed to improve cancer awareness in African American populations in both poor rural areas and urban areas of Alabama and Mississippi, and the CHAs are volunteer community members who have completed comprehensive training on cancer awareness (Hinton, Downey, Lisovicz, Mayfield-Johnson, & White-Johnson, 2005).
The study was designed to survey CHAs for two primary reasons. First, we are interested in adopting or adapting models such as the EFNEP and FSNEP paraprofessional model and the DSNCC Community Health Advisor Model to improve nutrition education communication strategies, to disseminate 2005 DG messages, and ultimately to reduce nutrition-related health disparities in hard-to-reach African American communities. Therefore, it was of interest to learn what this informed group of individuals, who have received previous health-related training, know about the 2005 DG. Second, these CHAs serve as a vital link between their communities and public health promotion efforts and reflect their communities' awareness, perceptions, and opinions concerning health and its broader social and cultural context.
The primary objectives of the research reported here were to describe the CHAs' own awareness of, knowledge of, and interest in receiving training regarding the 2005 DG and MyPyramid. Secondary objectives were to explore CHAs' insights into their communities' awareness of and knowledge of the 2005 DG and to investigate their communities' preferred communication channels for receiving messages promoting the MyPyramid. This data was collected in June of 2006, approximately 14 months after release of the 2005 DG in January of 2005 and the MyPyramid in April of 2005.
Methods
Survey Instrument
Because no known published research or standardized tool existed to measure awareness or knowledge of 2005 DG and MyPyramid, we developed an instrument. Content validity was established by an expert review panel including three doctoral-level Registered Dietitians and one DSNCC researcher. The panel gave feedback on the survey's content, clarity, and cognitive complexity.
The survey underwent a series of reviews through this process, resulting in several changes, including modifications in the question and answer choices, simplification of sentence structure, adjustments in overall flow and survey layout, and addition of a fifth answer choice to all knowledge questions to include "I don't know." Face validity was then established with a convenience sample of five CHAs who pilot tested the survey. They completed the written survey and responded to structured, interviewer-administered questions regarding clarity of questions, response categories, and the questionnaire format, flow, and length. Minor changes were then made to the wording of several questions.
The resulting 33-item survey included three sections: 1) nutrition awareness and knowledge, 2) community perspectives, and 3) demographics. In the nutrition awareness and knowledge section, participants were asked to indicate their awareness of the new 2005 DG, to rate their own perceived knowledge of the new 2005 DG, and to select from among four choices the most recent graphic promoted by the new 2005 DG. A series of 10 multiple-choice knowledge questions were asked, including one question each on the number of cups/ounces recommended for grains, fruits, vegetables, milk, meat, and beans, and one question each on recommendations for grams of fiber, percent calories from fat, types of healthy fats, percent of whole grains, and milligrams of sodium. The community perspectives section included six questions requesting the CHAs to rate their communities' awareness and knowledge of the 2005 DG, and make judgments on preferred and appropriate communication channels to promote the guidelines. Last, 10 demographic questions were included.
Data Collection
The research was approved by The University of Southern Mississippi's Institutional Review Board. Participants included CHAs from Alabama and Mississippi who attended the Annual Institute for the DSNCC in June of 2006 in Tuskegee, Alabama. A cover letter, consent to participate, and survey instrument were included in program packets distributed upon registration. The CHAs were approached at educational sessions and asked to complete the survey at their convenience and return the survey to a specified collection box. Upon returning the survey, CHAs were given the opportunity to enter a drawing to win one of two $50 gift cards.
Statistical Analysis
Descriptive statistics, including frequencies, percents, means, and standard deviations (SD), were used to examine survey responses. For the 10 knowledge questions, a composite score (ranging from 0-10) was determined for the total correct responses. Spearman's correlations were used to determine the relationships between: 1) confirming awareness of the new DG and correctly identifying the MyPyramid graphic, and 2) the perceived knowledge and actual knowledge of the 2005 DG. The item discrimination index correlates the score for each question with the total score and was used to evaluate reliability of the 10 knowledge questions. A value of 0.20 is the suggested criterion for item inclusion (Kline, 1993).
Results
There were 201 CHAs in attendance at the 2006 DSNCC Institute, and 106 completed the survey. Respondents were primarily African American (98%) women (90%). Approximately 65% had attended or completed college, and the average annual family income was approximately $28,000. Respondents represented 11 rural Alabama (Black Belt) counties, one urban Alabama county, one rural Mississippi (Delta) county, and two urban Mississippi counties.
When asked if they were aware that the government had announced new DG, 75 (71%) respondents indicated "yes." However, when asked to identify the most recent picture promoted by the new guidelines, only 16 (15%) respondents correctly identified the MyPyramid graphic. The majority (37%) identified the 1992 Food Guide Pyramid and 9% identified the Canadian Food Guide as the most recent graphic. The correlation between confirming awareness of the 2005 DG and correctly identifying the MyPyramid graphic was not significant (r=-0.09, p=0.47). When asked to identify all the ways they had heard or seen about the new DG, the most frequent responses were television (54%), CHAs meetings (40%), and brochures/pamphlets (39%). The response category chosen least was the Internet/WWW (10%).
Figures 1 and 2 illustrates the 10 knowledge questions and answer choices in the order presented on the survey instrument, along with the frequency of responses for each answer choice. Nine of 10 questions scored above the 0.20 item discrimination index, indicating high reliability. Only the whole-grains question received a lower score, at 0.17. Responses for individual knowledge questions ranged from a high of 62% of respondents correctly identifying the correct amount of milk recommended to a low of 9% of respondents correctly identifying the correct amount of sodium recommended by the 2005 DG. The actual knowledge average composite score was 3.4 (SD+1.6) out of a possible 10. When asked to rate their own perceived knowledge of the new DG on a 5-point Likert scale ranging from 1=poor to 5=very good, the average was 2.8 (SD+1.2). There was a significant correlation between perceived knowledge and actual knowledge of the 2005 DG (r=0.3, p=.002).
Figure 1.
Community Health Advisors Knowledge of the Cups and Ounces Recommended by the 2005 Dietary Guidelines (DG) and MyPyramid (n=106)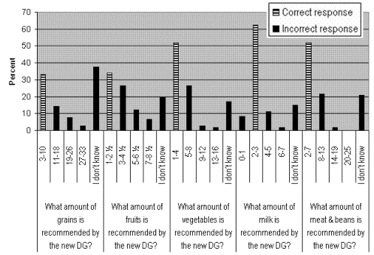
Figure 2.
Community Health Advisors Knowledge of Fiber, Fat, Grains, and Sodium Recommendations from the 2005 Dietary Guidelines (DG) and MyPyramid (n=106)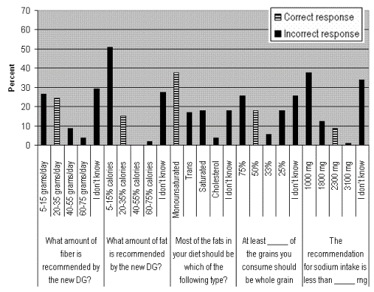
Next the CHAs were asked to make judgments about their communities' preference for receiving nutrition information. When asked to rank the preferred delivery format for promoting awareness of nutrition recommendations in their communities, the majority (43%) ranked television as number one, followed by the newspaper at 13%. Only 8% ranked the Internet as the number one preferred format. In a similar but separate item, a question was asked related to appropriate intervention approaches. The majority (54%) ranked activities the highest, followed by printed materials (25%), classes (22%), and videos (18%). Again the Internet was ranked lowest at 1%. When respondents were asked to rate their communities' knowledge of the new DG on a 5-point Likert scale ranging from 1=poor to 5=very good, the average was 1.9 (SD+1.0), with 44 (42%) responding 1=poor and 32 (30%) responding 2=fair.
Figure 3 describes how respondents rated their personal interest in the 2005 DG and judged their communities' awareness and knowledge of the DG on a 5-point Likert scale ranging from 1=strongly agree to 5=strongly disagree. Although there was not consensus on their communities' awareness of the 2005 DG, most respondents strongly agreed that they would like to know more about the DG (86%), more should be done in their community (81%), and their community would benefit from nutrition messages promoting the new DG (82%).
Figure 3.
Community Health Advisors' Views Regarding the 2005 Dietary Guidelines (DG) (n=106)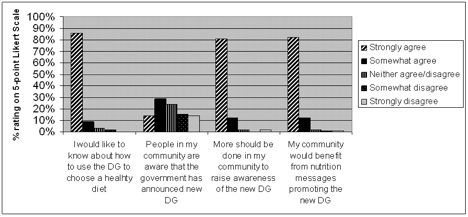
Discussion
Overall, the research reported here resulted in two very important findings. First, despite the CHAs' poor knowledge of the 2005 DG, it was important to discover that 86% expressed strong interest in learning more about nutrition recommendations. These individuals can provide communication and services within the cultural, linguistic, and other value systems of African American communities (Hinton et al., 2005; Kuhajda et al., 2006). Once they have been adequately trained, the CHAs have the enormous potential to help promote the MyPyramid within their hard-to-reach communities.
Because nutrition was not a core area of health education for the CHAs surveyed in the study, their nutrition knowledge scores are not expected to be particularly high. Nonetheless, the dismal knowledge scores are of concern because the survey questions represent the type of consumer-focused information promoted by the 2005 DG and MyPyramid, and these CHAs are regarded as knowledgeable health educators and role models. Perhaps the most alarming realization was that although the MyPyramid had been released for about 14 months at the time of this survey, only 15% of the CHAs were able to identify the MyPyramid graphic. It is theorized that awareness and knowledge of the 2005 DG and MyPyramid may be even lower among their non-CHA community peers.
Second, since little is known about Alabama's Black Belt and the Lower Mississippi Delta residents' media exposure and sources of nutrition-related information, the CHAs' insights regarding appropriate methods of communication and perceived lack of dissemination of the 2005 DG in these regions were extremely valuable. Although nationally the Internet is one of the most widely reported sources of health information, the CHAs indicated the Internet was not a preferred method of communication in their communities (Hesse et al., 2005). The Internet was ranked among the lowest choices for both the preferred delivery format for promoting nutrition recommendations in the CHAs' communities and for ways they had personally heard about or seen the new DG.
Although the Internet has become a useful tool for providing health information, there are access and usability challenges for low literate, low-income adults (Birru et al., 2004; Birru & Steinman, 2004). With the launch of the www.MyPyramid.gov Web site, the Internet appears to be the major communication channel used to disseminate personalized and detailed information regarding the MyPyramid. Nutrition educators have also been working hard to produce consumer handouts and brochures reflecting these new recommendations. However, these findings suggest MyPyramid messages and resources have not infiltrated the underserved communities in Alabama's Black Belt and the Lower Mississippi Delta region which lack Internet and health care access (Gamm & Hutchison, 2004; US Census Bureau). These research findings suggest that television is the most appropriate format to build awareness and that activity-oriented approaches should be used as an intervention strategy.
Because the study was conducted approximately 14 months after release of the 2005 DG and the MyPyramid, it is important to consider if this length of time was sufficient for the messages to be adequately disseminated. The field of health communication science has deliberated this type of issue, and it caries a multitude of considerations. For example, in communicating dietary messages a wide variety of factors affect dissemination, including mode of message delivery, intensity and duration of message delivery, and perplexity of the message, as well as motivation, social status, and health literacy level of the intended audience (Snyder, 2007; Hornick & Kelly, 2007; Viswanath & Bond, 2007).
Because our study was not designed to examine these other factors, it is difficult to thoroughly evaluate diffusion of the MyPyramid messages solely based on time frame. However, in a study we conducted approximately 24 months after release of the 2005 DG and the MyPyramid, dissemination of the messages still appeared very low, as only 12% of 177 community members residing in the Lower Mississippi Delta could correctly identify the MyPyramid (Zoellner, Connell, Bounds, Crook, & Yadrick, in press). Although actual knowledge scores were not measured in this study, when asked to rate their knowledge of the 2005 Dietary Guidelines on a 5-point Likert scale (with 1 = poor, and 5 = very good), the average was 1.8 ± 1.0, with the majority perceiving their knowledge as poor (53%) or fair (25%).
In summation of the health communication literature, there is agreement that health messages must be delivered repeatedly and over an extended timeframe for the messages to become rooted in communities. Cumulatively, the health communication literature and our data suggest that communication strategies promoting the MyPyramid messages are not sufficient to achieve optimal dietary intake.
The convenience sample of CHAs surveyed in the study may be viewed as a study limitation. Although a well known and established role of trained CHA is to represent the views and advocate for the needs of individuals and communities (Brownstein & Rosenthal, 1998; U.S. Department of Health and Human Services, 1994), only one known comparative validation study has explored the level of agreement between health workers report and community members self-report (Clough et al., 2002). Clough and colleagues examined illicit substance use and found very good agreement between health workers' report and community members' self-report history of kava use (k=0.77).
In our study, the degree to which the CHAs' personal perceptions influenced their answers regarding their community's perception is not known and should be accounted for in the interpretation of the study. However, it is feasible to suggest that these CHAs adequately represent the views of their communities and that therefore the results regarding community perspectives are generalizable to other populations in the southern Black Belt Region. This region refers to 623 counties located across parts of 11 southern states that are characterized by numerous inequalities, including rural decline, poor health, and inadequate education (Black Belt U.S. region). Although the awareness and knowledge findings may have limited generalizability to other groups, the study reported here lays the foundation to replicate the research in other populations. Future research is needed to explore the level of agreement between CHA responses and self-report from individuals among represented communities.
For nutrition educators and researchers, these findings suggest the importance of fostering collaborative relationships among the EFNEP or FSNEP and other programs that have established networks of community-based health educators. Both EFNEP and FSNEP have embraced a comprehensive paraprofessional training program, and FSNEP has developed competencies for paraprofessionals.
One of the central issues in the scientific literature regarding the use of community-based lay health educators for health-related interventions is the need to strengthen their training and evaluation components (Jackson & Parks, 1997; Rhodes et al., 2007). Established networks of community-based health educators could seek the expertise and guidance of EFNEP or FSNEP for nutrition-related training and evaluation, and EFNEP or FNSEP could partner with the community health networks as a means of improving the visibility of the 2005 DG and MyPyramid.
Resource limitations are consistently a problem for all programs, especially those challenged with addressing the multi-dimensional health needs of disadvantaged populations. There is a continued focus on decreasing health disparities as well as an ongoing need for cost-effective and culturally appropriate methods to reach at-risk, rural communities. Fostering collaborative relationships between EFNEP or FSNEP and other established networks of community-based health educators could be one innovative approach to access health disparity communities, maximize resource use, promote credible nutrition-related resources, and utilize culturally appropriate communication channels.
Conclusions
The community health advisors surveyed in the study reported here were very interested in learning about dietary recommendations, despite their inability to identify the MyPyramid graphic and their poor nutrition knowledge scores. The CHAs commonly indicated more should be done in their communities to promote the 2005 DG and indicated that the Internet was the least preferred method to communicate MyPyramid key messages. Relying on the Internet and other traditional health care communication channels to build awareness and disseminate MyPyramid key messages may be inappropriate and only widen the health disparity gaps in rural regions of Alabama's Black Belt and the Lower Mississippi Delta. There is potential for EFNEP and FSNEP to expand its outreach and efforts in improving the nutrition status of underserved, hard-to-reach communities by partnering within previously established networks of community-based health educators.
References
Adult Literacy Estimates. (1996). Retrieved October 7, 2005, from: http://www.casas.org/lit/litcode/Search.cfm
Birru, M., Monaco, V., Charles, L., Drew, H., Njie, V., Bierra, T., et al. (2004). Internet usage by low-literacy adults seeking health information: An observational analysis. Journal of Medical Internet Research, 6(3), e25.
Birru, M., & Steinman, R. (2004). Online health information and low-literacy African Americans. Journal of Medical Internet Research, 6(3), e26.
Black Belt (U.S. region). Retrieved September 15, 2006, from: http://en.wikipedia.org/w/index.php?title=Black_Belt_%28U.S._region%29&oldid=72511287
Brownstein J. N., & Rosenthal, E. L. (1998). The challenge of evaluating CHA services. In Rosenthtal E. L., Wiggins N., Brownstein J. N., Meister, J., Rael, R., de Zapien, G., et al., (Eds.), Report of the National Community Health Advisor Study (Chapter 4, pp. 50-74). Tucson, Arizona: Mel and Enid Zuckerman Arizona College of Public Health.
Burney, J., & Haughton, B. (2002). EFNEP: A nutrition education program that demonstrates costs-benefit. Journal of the American Dietetic Association, 102(1), 39-45.
Clough, A. R., Baille, R., Burns, C. B., Guyula T., Wunungmurra, R., & Wanybarrnga, S. R., (2002). Validity and utility of community health workers' estimation of kava use. Australian and New Zealand Journal of Public Health, 26(1), 52-57.
Dickin, K. L., Dollahite, J. S., & Habicht, J. P. (2005). Nutrition behavior change among EFNEP participants is higher at sites that are well managed and whose front-line nutrition educators value the program. Journal of Nutrition, 135, 2199-2205.
Dietary Guidelines for Americans. Retrieved June 01, 2006, from: www.health.gov/dietaryguidelines/
Gamm, L., & Hutchison, L. (Eds.). (2004). Rural healthy people 2010: A companion document to healthy people 2010. Vol. 3. Retrieved June 01, 2006, from: http://www.srph.tamhsc.edu/centers/rhp2010
Hardy, C., Wynn, T., Huckaby, F., Lisovicz, N., & White-Johnson, F. (2005). African American community health advisors trained as research partners: Recruitment and training. Family and Community Health, 28(1), 28-40.
Hesse, B., Nelson, D., Kreps, G., Croyle, R., Arora, N., Rimer, B., et al. (2005). Trust and sources of health information: The impact of the Internet and its implications for health providers: Findings from the first Health Information National Trends Survey. Archives of Internal Medicine, 165(22), 2618-2624.
Hinton, A., Downey, J., Lisovicz, N., Mayfield-Johnson, S., & White-Johnson, F. (2005). The community health advisor program and the Deep South Network for Cancer Control: Health promotion programs for volunteer community health advisors. Family and Community Health, 28(1), 20-27.
Hornick, R. & Kelly, B. (2007). Communication and diet: An overview of experience and principles. Journal of Nutrition Education and Behavior, 39(2S), S5-S12.
Jackson, E. J., & Parks, C. P. (1997). Recruitment and training issues from selected lay health advisor programs among African Americans: A 20-Year Perspective. Health Education and Behavior, 24(4), 418-431.
Kline, P. (1993). The handbook of psychological testing. London: Routledge.
Kuhajda, M., Cornell, C., Brownstein, J., Littleton, M., Stalker, V., Bittner, V., et al. (2006). Training community health workers to reduce health disparities in Alabama's Black Belt. Family and Community Health, 29(2), 89-102.
MyPyramid. Retrieved June 1, 2006, from: http://www.mypryamid.gov/
Rajgopal, R., Cox, R. H., Lambur, M., & Lewis, E. C. (2002). Cost-benefit analysis indicates the positive economic benefits of the expanded food and nutrition education program related to chronic disease prevention. Journal of Nutrition Education and Behavior, 34(1), 26-37.
Rhodes, S. D., Foley, K. L., Zometa, C. S., & Bloom, F. R. (2007). Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Medicine, 33(5), 418-427.
Snyder, L. B. (2007). Health communication campaigns and their impact on behavior. Journal of Nutrition Education and Behavior, 39(2S), S32-S40.
US Census Bureau. Retrieved March 15, 2006, from: http://www.census.gov/
USDA Cooperative State Research, Education, and Extension Service. Paraprofessionals Core Competencies. Retrieved November 7, 2007, from: http://www.csrees.usda.gov/nea/food/fsne/pdfs/paraprof_core_comp.pdf
US Department of Health and Human Services (USDHHS) (1994). Community health advisors: Models, research and practice, selected annotations- United States. Vol. 1. Atlanta GA: Division of Chronic Disease Control and Community Intervention, National Center for Chronic Disease and Prevention and Health Promotion, Centers for Disease Control and Prevention, Public Health Service, USDHHS.
Viswanath, K., & Bond, K. (2007). Social determinants and nutrition: Reflections on the role of communication. Journal of Nutrition Education and Behavior, 39(2S), S20-S24.
Zoellner, J., Connell, C., Bounds, W., Crook, L., & Yadrick, K. (in press). Seeking and trust of nutrition information is associated with nutrition literacy status among adults in the Lower Mississippi Delta. Preventing Chronic Disease.